The story I am about to tell is important on so many levels. First and foremost, it is a brief magnification of the journey of a man that I worked with as a counsellor who was struggling profoundly with an opiate dependence. I don’t think there are many other ways to describe that struggle except maybe formidable, terrifying, hopeless, desperate, soul betraying, the demon that eclipses true love and replaces it with lies.
The next thing Vince’s story tells us is how living in a safe and comfortable space is paramount to life. His story also helps tell us about how intolerance, and old ways and beliefs about substance use are not the answers to the struggles the person is suffering, especially in this age of the poisoning of street product. Placing sanctions on substance use alone and treating it solely as bad behaviour only serves to drive that behaviour underground and/or behind closed doors.
I mentioned the eclipse of love earlier and that is one of the most important messages of Vince’s story. Despite his challenges, his dependent coping mechanisms, his unfortunate loss of self control over his opiate addiction, he was very and most demonstrably capable of love. There were moments when his love would shine through his pain and soothe him until his demons would return.
There was more going on with Vince than just his addiction to IV opiates. He suffered from a personality disorder symptomatic of borderline personality disorder (BPD). This can be debilitating and life consuming for people who suffer with it. It has ways of confusing the person’s perception and experience of love and assists in the development of maladaptive coping habits like substance use. Overall it can be an extremely painful experience for the person and for those who love the person. It can show up as extreme selfishness, aggression and complete rages. It often shows up depression that can result in self harm and sometimes suicidal thoughts and attempts. So it is not hard to see why Vince was isolated from the ones that he loved. But that did not for one second kill his love for family, especially his young son.
Vince was referred to me by staff from the supportive housing he was residing at. They complained that they were finding drug paraphernalia such as unused needles and other packages and cookers etc., consistent with IV drug use. They were sincerely worried about him I’m sure. However, the policy of that housing at the time was 0 tolerance of substance use, possession of substances or paraphernalia anywhere within the building. Any violation of that policy could result in immediate eviction of the offender. Rather than evicting him right off the bat though, they thought if he received help for his addiction, then his addiction would be brought in check and he would be able to remain at the residence. As we will see, it is not as easy as all that.
It was a little difficult to get to know Vince. He was quite guarded and it took time for him to relax and for both of us to find our “groove” with each other so to speak. People with BPD can be inconsistent most of the time. They can seem like they are comfortable with you at one time and then apparently turn on you and be angry about something with you at another time. With BPD emotions do not necessarily have a “thermostat” to regulate the level of feeling the person is experiencing so sometimes, our sessions were quite intense. I would, at times, walk out after a visit feeling quite drained. Working with someone with this disorder requires a great degree of patience, empathy, compassion, and very healthy boundaries. Regardless though, our relationship grew and we were able to address the issues at hand.
Vince’s main goal was to reconnect with his son. At the time that we had met, he was not allowed any contact with his son at all. His separation from his partner, as you might imagine, was rife with anger and conflict and as a result, the Ministry of Child and Family Development was barring Vince from having contact with is son. The reasons; his substance use and his anger. Rightly so at that time I have to say. Regardless, he was bound and determined to reconnect with his son. Our main strategy was to work on his IV opiate dependence.
I will make a very long story shorter. There was certainly a lot of inner work that we did working on alternative coping strategies. We worked on relaxation and distraction exercises for example with distraction being the most effective for Vince. Relaxation only seemed to work when things were relatively stable for him which was okay as there is no bad time to practice relaxation. We definitely focused on his love for his son. Motivation is the foundation of recovery in my opinion and Vince had no shortage of that. Like I said, when he was well and stable, his love was overflowing.
Fortunately, strategies for recovery from addiction and for BPD (and many other disorders) are almost identical. That is no surprise as substance use addiction is considered a mental health disorder. We also employed a medical intervention as Vince agreed to access the methadone program at that time. In short, methadone is an opiate replacement therapy that, at the right dose, curbs cravings for opiates. Eventually, Vince reported that his IV use had ceased. There was no visible evidence to dispute his reports. He eventually won the ability to have supervised visits with his son and obtained a part time job. His enthusiasm and passion for life appeared to be growing in leaps and bounds. Everyone was satisfied and happy….until..
I am not sure what triggered the relapse. We know that relapse occurs with up to 95% of people who use opiates. I say relapse as that is one of the typical times that an overdose will occur. It was likely being laid off of work and the slow pace of his progress with visitations with his son. Remember that his emotional thermostat was still broken or non existent and he was still prone to emotional outbursts, extreme agitation or depression. This, in my opinion, was why he was using in the first place.
None of us know the intimate, all encompassing comfort and the warmth of the hug that those who use opiates experience. I am sure my words do not even reach the deepness of the experience that I hear about so often. I have experienced my own “warm hug” with alcohol but I would not pretend that it would be the same. This warm hug instantly relieves any pain the person is experiencing as it’s supposed to do. It is not the “party” high that people think it is; at least not for those who suffer from the disorder. Vince likely stopped using his methadone, or maybe missed an appointment or whatever and then defaulted to his old ways of dealing with his moods and circumstances. Regardless of why, it happened. He overdosed in his suite.
That was not the end. Staff found him on time, laying on his floor amongst scattered needles and other paraphernalia. He spent some time in hospital and was released just a couple of days afterwards. When he arrived back at his suite, the eviction letter was waiting for him. Zero tolerance. No more chances. Vince was obviously extremely upset about this and started to push everyone away, including me. He lost his visits with his son. He continued to use. He ended up homeless for a short time and stayed at the Gospel Mission before he was eventually able to find a small place accompanied by a roommate. He was constantly in our clinic for harm reduction supplies so we knew he was still in the throes of his addiction.
About four months after his eviction, he was found unresponsive in his apartment by his roommate. He did not make it. Vince fell victim to the onset of the poisoning of the illicit supply of heroin that was beginning to sweep our community at that time. The poisoning would claim well over 50 of my clients over the next 6 years, so many I stopped counting after three years. Father and son would never meet again. His family and his roommate were devastated. I went in to a depression, brief but intense. Vince was one of too many who’s story I knew at an intimate level. The loss was not unlike losing a close friend.
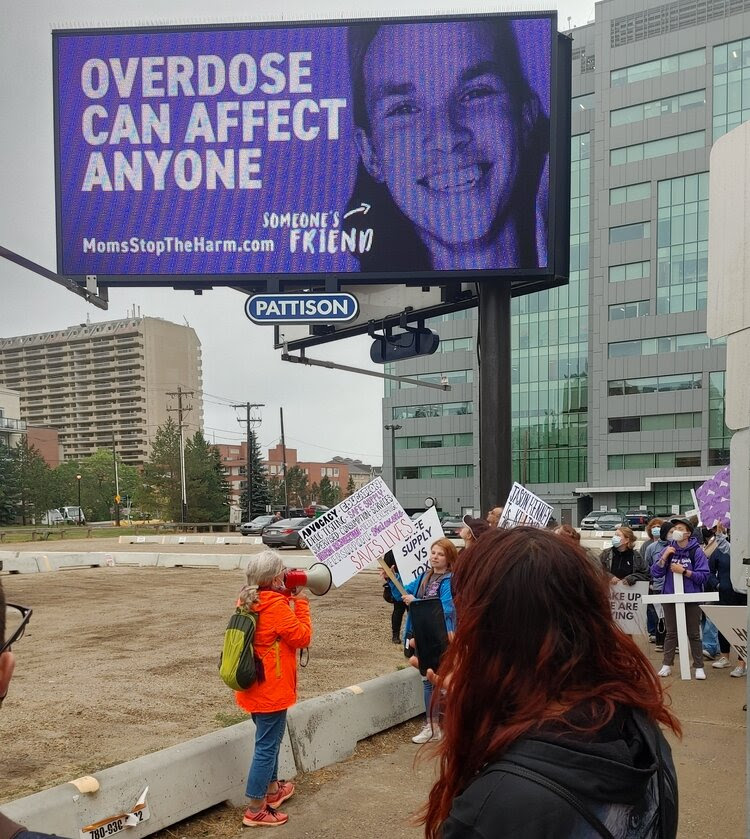
The onset of the poisoning of the illicit supply of heroin and other stimulants as well, grew and grew. It was first and is still identified as the overdose crisis. But we know that the majority of people who have overdosed and survived did not know there was fentanyl or carfentanyl in their product. To date well over 30,000 deaths have been reported in Canada from this poisoning since 2016.
One of the responses to the poisoning was a significant change in policies at supportive housing facilities. You see, I was not the only person in the field experiencing massive losses to this crime. People like Vince have always used in their rooms despite the sanctions and consequences. It was a better alternative than in an alley or some bathroom somewhere. People have mostly used alone as well because of the illegality of possession, not just of drugs but also paraphernalia. So people choose to use in the relative privacy and safety of their own homes. Unfortunately this turned into one the most dangerous practices and remains so today for substance users.
Residential workers were becoming overwhelmed and over traumatized by walking in on overdoses and, horrifically, dead bodies. It seems like every month for a while our supportive residences were reporting deaths due to overdose. This had been a very rare occurrence before the crisis grew. So eventually, and very quietly, so the uninformed community would not lose its mind, the facilities, including the one where Vince had lived, developed harm reduction strategies that would soon see a significant reduction in fatalities within these residences.
They changed their policies from 0 tolerance to harm reduction. They established safe injection/using rooms in their buildings and offered harm reduction supplies. Monitoring protocols were offered with tenants so that staff were actually aware of when someone would use and would check on them periodically to ensure safety. Many more people who are no longer subjected to sanctions and intolerance are now more actively seeking out help.
Two things got in the way though. Stigma and lack of resources. Stigma still is a main barrier that contributes to using alone. Just because policy has changed, attitudes are much slower to to do so. We tend to rely on our familiar beliefs rather than change.
Of course, it takes more staff to monitor this and funding is almost non existent. So while the potential to reduce even more harm is possible, it is stymied by lack of resources and the broken promise of “wrap around services”.
There has been very little if any negative impact on communities as a direct result of this policy though. Despite the facts, some people in the community still operate from a place of stigma.
Despite the challenges we still face, imagine if harm reduction and flexible tolerance had been already in place for Vince. His son would likely still have his father, despite his father’s challenges. People like myself could still be working with Vince supporting him in helping to stabilize his life. There are multiple options for opiate replacement therapy now including a slowly growing access to safer supply and the helping community has evolved to embrace harm reduction as a step towards recovery…at least many programs have. There are still too many traditional 0 tolerance programs that actually put people at more risk of overdose.
Regardless, many of the deaths that have occurred could have been prevented if we as a society would change how we see substance use disorder. Imagine today, if harm reduction did not exist. How many more memorials and celebrations of life we would need to attend? If we could only see the people first and not the illness, maybe we could save lives. If anything, follow this mantra: Compassion not punishment.
Vince responded to compassion, healthy boundaries, respect and dignity. When they were taken from him, he fell back to his default coping.
You can reach me at bengoerner.bg@gmail.com or leave a comment below.